Incontinence, is it a normal part of aging?
What is incontinence?
Incontinence is the involuntary loss of bladder an bowel control. - Continence Foundation of Australia
Key statistics of Incontinence in Australia - The Continence Foundation of Australia
Over 5 million Australians – 1 in 4 people aged 15 years or over – experience bladder or bowel control problems. This number is predicted to grow to 6.5 million by 2030.
80% of people with urinary incontinence are women.
1 in 3 women who ever had a baby wet themselves.
Strong pelvic floor muscles are necessary for bladder and bowel control.
Pelvic floor muscle exercises have been shown to prevent and treat incontinence at any age.
Less than 2 out of 10 women (17.6%) do their pelvic floor exercises daily.
70% of incontinent people do not seek help.
Bladder and bowel control problems are not a natural part of ageing or having a baby.
Incontinence can have long-term physical and emotional impact; affecting self-esteem, motivation and independence.
Who is at risk?
Incontinence doesn’t discriminate
Incontinence affects women, men and children of all ages, physical ability and background. There are however some health conditions and life events that can put you at an increased risk of developing either urinary or faecal incontinence.
Urinary incontinence risk factors
Risk factors commonly linked with urinary incontinence include:
pregnancy (both pre- and post-natal women)
younger women who have had children
obesity
urinary tract infections
specific types of surgery such as hysterectomy (removal of all or part of the uterus and/or ovaries)
reduced mobility preventing you from getting to or using the toilet
neurological and musculoskeletal conditions such as multiple sclerosis and arthritis
health conditions such as diabetes, stroke, heart conditions, respiratory conditions, and prostate problems, and
some medications.
Faecal incontinence risk factors
A risk factor for faecal incontinence is urinary incontinence. Other risk factors are similar to those of urinary incontinence, but also include:
There are 4 types of urinary incontinence, namely:
Stress incontinence
Urge incontinence
Chronic retention or overflow incontinence
Functional incontinence
Nocturia
Stress Incontinence
‘Common causes
Stress incontinence is most common with activities such as coughing, sneezing, laughing, walking, lifting, or participating in sports such as gym and weight lifting.
Other factors that contribute to stress incontinence include diabetes, chronic cough (linked with asthma, smoking, bronchitis and some medications), constipation and obesity.
Stress incontinence in women may be caused by pregnancy, childbirth and menopause.
Pregnancy and childbirth can stretch and weaken the pelvic floor muscles that support the urethra (the bladder outlet tube) causing stress incontinence during activities that push down on the bladder.
During menopause, oestrogen (a female hormone) is produced in lower quantities.
Oestrogen helps to maintain the thickness of the urethral lining to keep the urethra sealed after passing urine (much like a washer seals water from leaking in a tap). As a result of this loss of oestrogen, some women experience stress incontinence.
2. Urge incontinence
Urge incontinence is the involuntary loss of urine (wee) associated with urgency (a sudden and strong need to urinate).
Our bladder can hold up to 600mls of urine. As our bladder fills with urine, it expands. When the bladder is half full you may need to the toilet to empty your bladder.
People with urge incontinence feel as if they are going to have an accident, and need to go to the toilet, even though their bladder isn’t full, often not making the toilet.
What causes urge incontinence?
Urge incontinence seems to become more common as we age. Symptoms may get worse at times of stress and may also be worsened by fluids like tea, coffee, fizzy drinks or alcohol.
Urge incontinence can be linked to stroke, Parkinson's, multiple sclerosis and other health conditions that interfere with the brain's ability to send messages to the bladder via the spinal cord. These conditions can affect a person's ability to hold and store urine.
Urge incontinence may also occur as a result of constipation, or simply the result of a long history of poor bladder habits such as going to the toilet before the bladder is full ("just in case"). In some cases, the cause of an overactive bladder is unknown.
Management options available
The aim in managing urge incontinence is to improve control of your bladder by:
reducing the strong urge sensation
gradually increasing the storage capacity or size of your bladder
increasing the period of time between visits to the toilet.
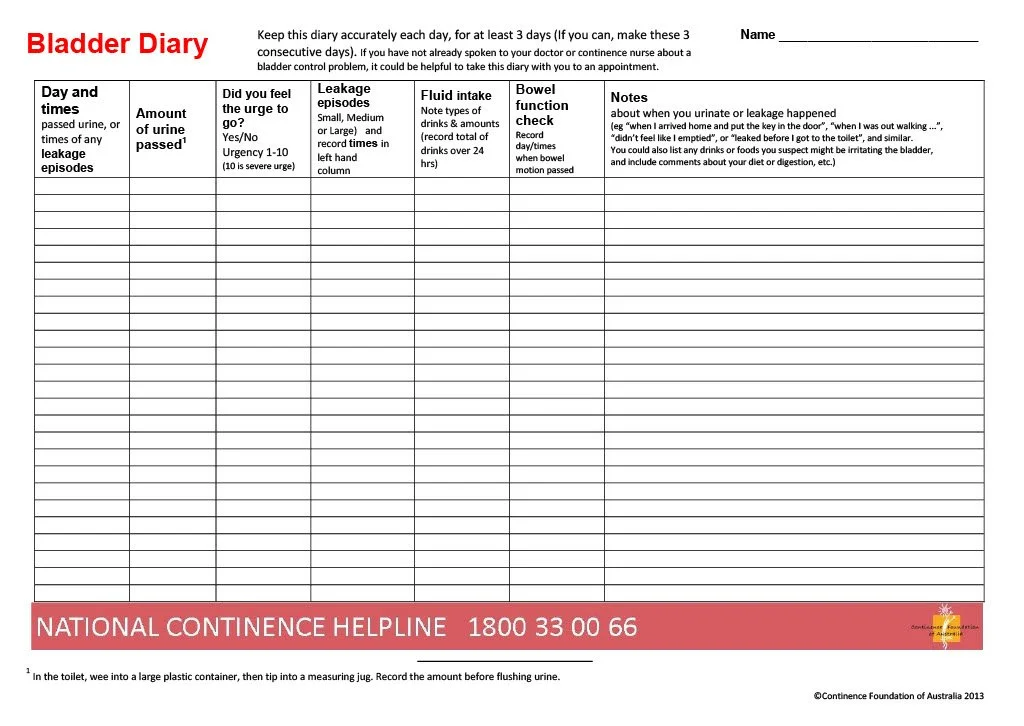
A bladder diary can help you to identify your pattern of passing urine and when accidental leakage is likely to occur. If you have not seen a doctor it may be useful to take this along to your appointment.
To download your copy of this Bladder Diary pdf, click here.
A bladder training program can help improve your bladder control. There are also specific prescription medicines that relax the bladder muscle and may improve the success of a bladder training program.
Having strong pelvic floor muscles will also help you to reduce urgency and help you hold the urine in the bladder until you get to the toilet.
3. Urinary retention
‘Urinary retention is when the bladder is unable to empty properly. With chronic retention you may leak small amounts of urine when there’s increased pressure on the bladder (e.g. while coughing, sneezing or opening the bowels).
Signs that your bladder is not completely emptying include:
feeling that you need to strain to pass urine
a weak or slow urine stream
feeling as if your bladder is not empty just after going to the toilet
little or no warning when you need to pass urine
passing urine while asleep
frequent urinary tract infections or cystitis
'dribbling' more urine after visiting the toilet.
Causes
There are several possible causes for this type of incontinence. These include:
A blockage of the urethra (bladder outlet tube) caused by a full bladder – the full bladder can put pressure on the urethra, making it difficult to pass urine
a prolapse of pelvic organs which can block the urethra
damage to the nerves that control the bladder, urethral sphincter or pelvic floor muscles
diabetes, multiple sclerosis, stroke or Parkinson's – these conditions can interfere with the sensation of a full bladder and with bladder emptying
some medications including over the counter medications and herbal products.
4. Functional incontinence
‘Disability Associated Urinary Incontinence
Disability associated urinary incontinence is defined by the International Continence Society (ICS) as urinary incontinence in the presence of a functional inability to reach a toilet in time. This may occur in those living with a physical or cognitive condition which may impact their ability to access the toilet.
Disability associated urinary incontinence is when a person is unable to:
recognise the need to go to the toilet
locate the toilet
access the toilet
manage their personal needs (e.g. remove clothing)
recognise the toilet.
Causes
When someone has disability associated urinary incontinence, it often means there is a physical, intellectual or environmental issue that makes it difficult for them to use the toilet.
Some of the causes of disability associated urinary incontinence include problems with walking (arthritis or cerebral palsy) and problems with memory or learning (such as dementia and intellectual disability).
For tips for carers click here.
5. Nocturia
Nocturia is when you wake up during the night or main sleep time because you have to pass urine (wee). It is a common problem that becomes more common as we get older.
Causes
Nocturia can be part of many common medical conditions, such as:
heart problems
kidney problems
poorly controlled diabetes (Type 1 or Type 2)
swollen ankles
taking fluid tablets at night for bladder infections
constipation as a full bowel can press on the bladder
an enlarged prostate as this may not let the bladder empty out fully.
Other things that can lead to nocturia are
being pregnant
changing your position from upright in the day to lying flat at night – this increases blood flow to the kidneys and more urine is produced
having broken sleep as you may go to the toilet just because you are awake
consuming large amounts of fluid before going to bed at night
consuming alcohol or caffeine (e.g. coffee, chocolate and cola) before going to bed at night.
Tips for managing nocturia include:
cutting back on caffeine and alcohol – especially in the evening and before going to bed
reviewing the times you take fluid tablets
resting with your legs up for a few hours in the afternoon or evening.
lighting the path to the toilet
placing a commode or urinal to use next to your bed.
Your doctor may refer you to a Nurse Continence Specialist, continence physiotherapist or medical specialist to discuss other treatments with you. This may include medications to treat the nocturia or the underlying cause.
SEEK HELP
Chronic urinary retention needs urgent professional help
Incontinence associated with chronic retention may cause serious damage to the bladder and kidneys and should always be treated by a doctor or continence health professional.
For further information and to find assistance in your area contact the National Continence Helpline on 1800 33 00 66. The National Continence Helpline is staffed by Nurse Continence Specialists who offer free and confidential information, advice and support. They also provide a wide range of continence-related resources and referrals to local services.
What is a normal healthy bladder?
The Incontinence Foundation of Australia states that a healthy bladder -
empties 4-6 times each day
can hold up to 400-600ml of urine (the sensation of needing to empty occurs at 200-300 ml)
may wake you up once at night to pass urine and twice if you are older (i.e. over 65 years of age)
tells you when it is full but gives you enough time to find a toilet
empties completely each time you pass urine
does not leak urine.
The Incontinence Foundation of Australia states that in many cases, incontinence can be prevented with a healthy diet and lifestyle habits.
Their other suggestions are:
Diet
Drink enough water to quench your thirst and spread your drinks out throughout the day.
Avoid reducing your liquid intake as this will concentrate your urine, making any bladder problem worse.
Practice good toilet habits
Go to the toilet when you get the urge and not ‘just in case’.
I have seen this so often that when arriving at a mall, women look out around for the loo and then go ‘just-in-case’. Unfortunately this teaches the bladder to ‘go’ even when it’s not full.
Visit your doctor as soon as you suspect a urinary tract infection.
Lead a healthy lifestyle
Be active by aiming at least 30 minutes of exercise most days.
Stop smoking.
Do your pelvic floor muscle exercises regularly.
The pelvic floor muscles
Just as you would exercise your arms and legs, you should also exercise your pelvic floor muscles regularly.
The Incontinence Foundation of Australia further states that in almost all cases it’s possible to gain control over the pelvic floor muscles and to train them to do their job well.
They also state that the pelvic floor muscle exercises can help with:
‘improving bladder and bowel control
reducing the risk of prolapse (in women)
better recovery from childbirth and surgery (in women)
better recovery after prostate surgery (in men)
increased sexual sensation
increased social confidence and quality of life.’
strengthening the pelvic floor muscles is important to help control the flow of urine.
To find out how to exercise the pelvic floor muscles, the Continence Foundation of Australia has produced this video showing how. If you need help with your pelvic floor muscles, please reach out, I would love to help you in a no stress, fun and easy way.
Incontinence doesn’t have to stop you from living your life. With a little planning, whether you are at home, work or travelling, consider these strategies.
If you are trying new strategies, try them out at home first before attempting them away from home.
If you are going out, know how long you are going to be out for.
Know where the nearest toilet is. ‘Download a public toilet map, which shows the location of more than 19,000 public and private public toilet facilities across Australia’.
4. If you know that you are prone to having ‘accidents’ when out and about, have enough incontinence products with you, a change of clothing, if necessary, wet wipes or odour neutralising products and a zip lock packet to keep the soiled clothing in.
Find help
Never ever think that you have to struggle on your own. Having a weakened pelvic floor is more common than you think and nothing to be embarrassed about.
Ask your doctor about help for bladder problems, as the symptoms will not go away on their own and may worsen over time or contact the National Continence Helpline on 1800 33 00 66. As previously mentioned, I am here if you need help. Just reach out.
The National Continence Helpline is staffed by Nurse Continence Specialists who offer free and confidential information, advice and support. They also provide a wide range of continence-related resources and referrals to local services.
Resources:
https://www.nia.nih.gov/health/urinary-incontinence-older-adults
https://www.health.gov.au/resources/publications/pelvic-floor-muscle-training-for-men